
Audit News
Q2.2024
Audit Question of the Month
How do I know when to submit a DAW 9 on a claim?
Your pharmacy may have seen messages when submitting prescription claims that say, “Plan prefers brand name, submit with DAW 9.” This is a common claim rejection or message pharmacies may receive on a claim adjudication. If you receive this message from the PBM plan, submit a DAW 9 on the claim and note your hardcopy as “DAW 9-plan prefers brand.”
It’s important to note a DAW 9 should never be used if you did NOT receive this message from the plan, even on refills for the same prescription number and medication. Many PBMs have been recouping claims amounts from pharmacies submitting a DAW 9 without the plan prompting for it—many PBMs will not accept any appeals to overturn the recoveries on an audit because, according to the PBM, “the pharmacy did not receive a claim message or rejection to submit the DAW 9, and did not contact the PBM pharmacy help desk before submitting the DAW 9.”
We suggest that if you have received a prompt or message from the PBM plan to submit DAW 9 on a claim and the refills do not have that same message, then you should contact the PBM’s pharmacy help desk to make sure the DAW 9 can still be submitted for this medication before taking any other action.
Audit Tips & Tricks
Audits for Medications That Must be Dispensed in Their Original Packaging
The RxProtect team has seen a recent increase in audits for medications that must be dispensed in their original packaging or container per their manufacturer. Many PBMs have started targeting claims where the pharmacy dispensed a prescription outside how medications are commercially available.
Medications most frequently on these audits include:
- Creon®
- Zenpep®
- Linzess®
- Most HIV medications
For example, Creon comes in bottles of 70, 100, and 250 capsules. If a pharmacy submits a claim for a quantity of 175 capsules, it could be flagged for a PBM audit.
Additionally, if the manufacturer’s package insert specifies the medication must be dispensed in its original packaging, then it cannot be placed in a pharmacy medication vial, bottle, or unit dose package.
RxProtect recommends ensuring prescriptions match commercially available quantities and dispensing in the manner listed on package inserts to avoid being flagged in a PBM audit. If quantities need an adjustment, obtain prescriber approval and document changes on the prescription to ensure compliance when dispensing to patients.
If you are unsure of a product’s specific requirements, you can look at the product’s package insert or go to DailyMed (nih.gov) to search for the product and view the FDA’s Product Dispensing Requirements.
Experiencing an Audit?
We can help! Contact our RxProtect team:
844-ALIGNRX (844-254-4679), option 2
rxprotect@alignrx.org
REMS of the Month: Jynarque®
Jynarque is used to slow kidney function decline in adults who are at risk for rapidly progressing autosomal dominant polycystic kidney disease (ADPKD).
- Generic Name: Tolvaptan
- Company: Otsuka
- Indications: Jynarque is used to slow kidney function decline in adults who are at risk for rapidly progressing ADPKD.
- Warnings: Risk of serious liver problems that can lead to the need for a liver transplant or can lead to death.
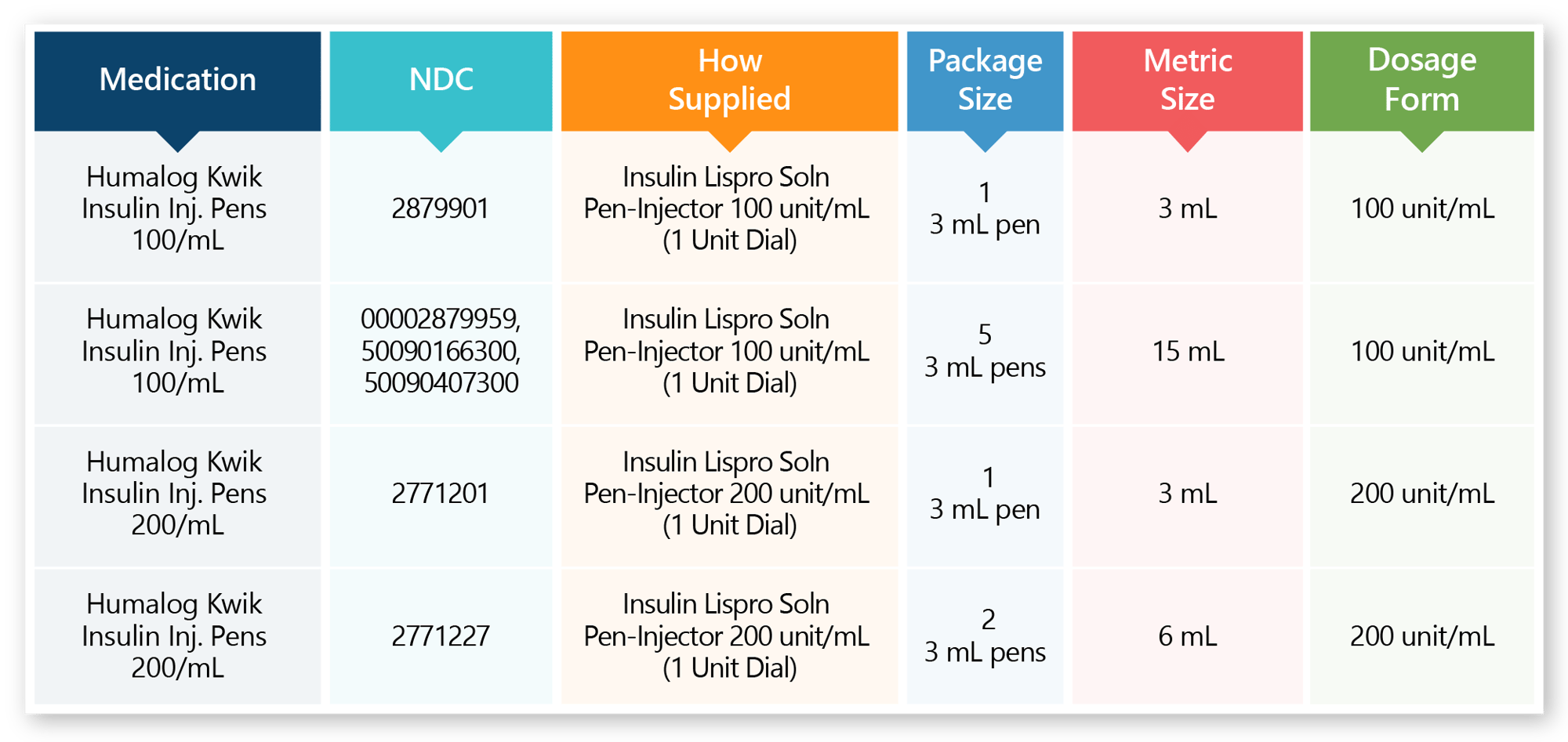
Drug Setup of the Month
Humalog KwikPens

Weekly Claims Report
RxProtect provides pharmacies with weekly reports that identify claims from the previous week that may be at risk of an audit. Remember to check your weekly RxProtect email for a link to access your pharmacy’s report. It is crucial for these reports to be reviewed on a weekly basis in order to have time to reverse and resubmit any errors when necessary. This is a proactive way to prevent an audit recovery! If your claims and documentation are correct, PBMs will find no reason to recoup money in a future audit.
Please note: Our weekly report can only show potential errors, as prescription directions are not transmitted on claims data, and RxProtect does not have access to images of your prescription hard copies. We can only flag claims with the highest audit risk, as PBMs will target them should you be audited.
Technician Training Available for RxProtect Members
RxProtect offers technician training for hard copy documentation requirements and billing guidelines. The training educates technicians on preventing audit recovery by providing key documentation requirements for prescriptions. It also guides technicians through proper billing techniques, which are necessary to prevent charge backs from PBMs. Technician training is available to all pharmacies enrolled in RxProtect.
To request training for your employees, please call 844-ALIGNRX (844-254-4679), option 2, or email rxprotect@alignrx.org.
Aberrant Product List from Caremark
As a reminder, Caremark monitors pharmacies each month for billing volume of NDCs on the Aberrant Product List. If, in one month, any one or combination of products on the Aberrant Product List accounts for 25% of the pharmacy’s claims or dollars (as measured by Caremark), the pharmacy will be in breach of the contract provision shown below. Caremark plans to make updates and regular changes to the Aberrant Product List and will communicate these changes through its pharmacy portal.
“Providers must not dispense aberrant quantities of a Covered Item and/or high volume of claims within a therapeutic category (e.g., topicals, dermatologicals), as measured by the number of claims, quantity dispensed or dollars, inconsistent with the habits of local Prescribers or Plan Sponsor formularies, at Caremark’s sole determination. In the event a Provider breaches this provision of the Provider Manual, Caremark, on its behalf, or on behalf of a Plan Sponsor, may terminate the Provider Agreement (or Provider’s participation in specific Plans or networks), and may exercise other remedies available to Caremark, including charge back of applicable claims.”
Pharmacies will receive notice from Caremark indicating a breach has occurred. Pharmacies will then have 30 days to cure the breach if they wish to continue their participation as a provider with Caremark. If a pharmacy breaches this contract provision at any time after the 30-day cure period, the pharmacy will be subject to termination and other remedies available to Caremark, including charge back of applicable claims.
The most recent additions to the Aberrant Product List can be found on the AlignRx Member Portal. Look for a link in the banner on the RxProtect page labeled, “Aberrant Product List New Additions.”




